Why Should I Choose a Mohs Surgeon Over a Dermatologist?
Choosing a Mohs Surgeon: What Qualifications Actually Matter?
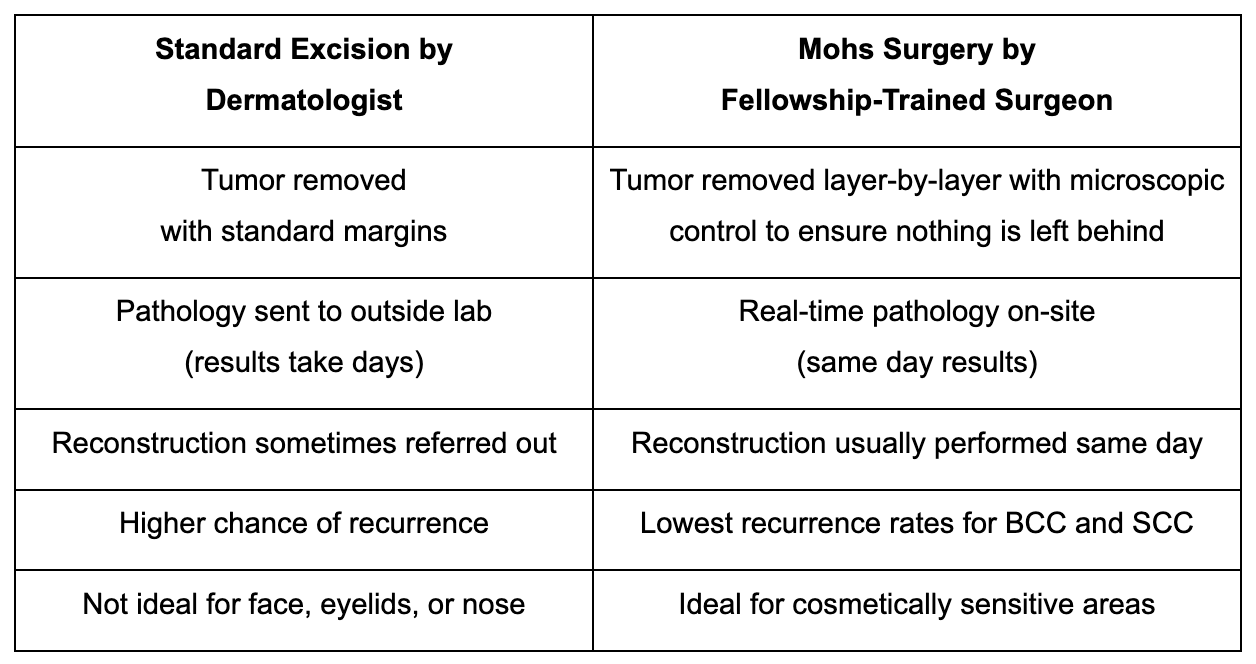
Skin cancer is an unfortunate reality that 1 in 5 Americans will confront in their lifetime. It’s a frightening battle but it’s one we must meet with action and awareness. This is why seeing a Mohs surgeon is a necessity for getting the most effective treatment available.While board certification is important, it doesn’t guarantee the highest level of surgical skill and expertise for skin cancer removal, especially in delicate, cosmetically sensitive areas like the face, nose, or eyelid. This is where fellowship training in Mohs surgery makes a big difference.This article will explore what Mohs micrographic surgery is, why it offers the highest cure rate for basal cell carcinoma and squamous cell carcinoma, and why choosing a fellowship-trained Mohs micrographic surgeon over a standard board-certified dermatologist is critical for the best cosmetic and surgical outcomes.
Understanding Mohs Surgery
Mohs micrographic surgery is a highly advanced and precise surgical method that removes skin cancer one layer at a time, with each layer carefully examined under a microscope using prepared slides. During the procedure, different forms of tissue are analyzed to identify symptoms such as skin sores, growths, and called lesions on the skin's surface. Mohs surgery is the gold standard for treating: Basal Cell Carcinoma (BCC), Squamous Cell Carcinoma (SCC), and High risk or cosmetically sensitive areas, such as the nose, ears, lips, eyelids, hands, and scalp
Mohs surgery is effective for various types of skin and different forms of skin cancer. It targets cancers that appear as lesions of various shades, including brown, on the skin's surface.
Why Mohs Surgery Is Considered the Best Skin Cancer Treatment
- Highest cure rate (up to 99%)
- Helps the skin heal with minimal scarring
- One of the most effective treatments for skin cancer
- Preserves healthy tissue
- Extremely fast tumor removal and reconstruction.
Why Being a Board-Certified Dermatologist Isn't Always Enough
1. Mohs Surgeons Are Also Skin Cancer Pathologists
A standard board-certified dermatologist is trained in diagnosing and treating a wide range of skin conditions. However, Mohs surgery also requires the ability to:
- Remove cancerous tissue layer by layer
- Prepare and analyze pathology slides in real time
- Accurately identify cancer cells under a microscope
- Make immediate surgical decisions based on pathology results
Examples of pathology techniques and diagnostic methods used during Mohs surgery include frozen section histology, staining procedures, and microscopic examination of tissue margins to ensure complete cancer removal.
A significant advantage of seeing a Mohs fellowship-trained surgeon is that their training in dermatopathology allows them to examine the tissue immediately and confirm that all cancerous cells have been removed, eliminating the need to wait days for an off-site pathology report.
2. Mohs Fellowship Surgeons Are Reconstructive Experts
Once the Mohs micrographic surgeon is assured of the complete removal of skin cancer through careful, step-by-step histopathological assessment, reconstruction of the surgical defect becomes the next priority. This is of critical importance when surgery involves areas of the body that are both aesthetically and functionally sensitive, such as the face or eyelid, where even minor imperfections can have significant repercussions on appearance as well as on vital functions like vision, speech, or breathing. Some of these sensitive areas, such as the eyelid or nose, are considered organs, making precise reconstruction essential for both organ function and appearance. Reconstruction in these regions requires a high degree of surgical precision, aesthetic judgment, and a thorough knowledge of intricate facial anatomy.
A fellowship-trained Mohs surgeon is uniquely qualified to perform these delicate reconstructive procedures, having undergone subspecialty training that extends beyond tumor excision to include advanced reconstructive methods. This equips them with expertise in local tissue rearrangement, skin grafting, and layered closures designed to restore natural facial contours while simultaneously reestablishing function. In the periocular region, for example, they are skilled in reconstructing the delicate architecture of the eyelid to protect the eye and preserve vision. On the nose, lips, and ears, they carefully balance symmetry, contour, and function to achieve a natural appearance while maintaining airway or oral competence.
It is this convergence of oncologic precision and reconstructive artistry that distinguishes fellowship-trained Mohs surgeons. By blending technical mastery with aesthetic sensitivity, they are able to provide patients with both the highest cure rates and the most optimal cosmetic and functional outcomes.
- Skin flap surgery
- Skin grafting
- Cosmetic reconstruction
- Scar minimization techniques
A general dermatologist without Mohs fellowship training does not have the surgical expertise to achieve optimal cosmetic results.
3. Fellowship-Trained Mohs Surgeons Undergo Extensive Training
To become a Mohs micrographic surgeon, a dermatologist must go beyond and complete:
- 3 years of dermatology residency
- 1 additional year of fellowship training in an ACGME or ACMS accredited Mohs surgery program
- Participate and gain hands-on experience with thousands of Mohs procedures
- Comply with the rigorous standards set by the American College of Mohs Surgery (ACMS)
This advanced training bridges the gap between pathology and clinical medicine, ensuring Mohs surgeons are equipped with the expertise needed for accurate diagnosis and effective treatment.
Mohs fellowship surgeons are trained to diagnose and treat a wide range of skin diseases, with a high-level focus on the diagnosis, removal, and reconstruction of skin cancer.
Advanced Diagnostic Capabilities: Precision in Identifying and Treating Skin Cancer
The landscape of skin cancer diagnosis and treatment has advanced dramatically, offering patients greater precision and better outcomes than ever before. When it comes to identifying and treating skin cancers such as squamous cell carcinoma and basal cell carcinoma, early and accurate diagnosis is critical. Squamous cell carcinomas often present as flat, reddish, or brownish patches with rough, scaly, or crusted surfaces, typically appearing on skin exposed to the sun—like the face, neck, lips, and hands. Basal cell carcinomas, the most common type of skin cancer, usually develop on sun-exposed parts of the body and may appear as raised, pale, pink, or red areas, sometimes with visible blood vessels.
A variety of factors can increase the risk of developing these skin cancers. Prolonged sun exposure, a weakened immune system, older age, and a family history of skin cancer all play significant roles. Most basal cell carcinomas and squamous cell skin cancers are highly treatable when detected early, but if left untreated, they can grow, invade other tissues, or even spread to other parts of the body, including lymph nodes and vital organs. This is why regular check-ups and early intervention are so important, especially for those with a history of sun exposure or weakened immune systems.
Modern diagnostic techniques, such as molecular pathology, have revolutionized the way doctors and surgeons identify abnormal cells and diagnose skin cancers. By examining molecules within skin cells and tissues, molecular pathology allows for a more accurate and timely diagnosis, ensuring that even subtle or early-stage skin lesions are detected. Clinical dermatology also plays a vital role, with many doctors recommending routine skin exams to catch suspicious growths or changes in the skin’s surface before they become more serious.
Other skin cancers, such as melanoma, can be life threatening if not diagnosed and treated promptly. Melanoma has the potential to spread to other parts of the body, including lymph nodes, making early detection and treatment essential. Pre-cancerous conditions like actinic keratosis and Bowen disease can also develop into squamous cell carcinoma if not addressed, underscoring the importance of vigilant medical care.
Treatment options for skin cancer depend on the type, location, and stage of the disease. Surgery remains the gold standard for many cases, but medicines and other therapies may also be used. Preventive measures, such as using sunscreen, seeking shade, and wearing protective clothing, are crucial in reducing the risk of developing skin cancer. Doctors and surgeons work together to provide comprehensive care, from diagnosis to treatment and follow-up, ensuring the best possible outcomes for patients.
Ultimately, advanced diagnostic capabilities have made it possible to identify and treat skin cancers like squamous cell carcinoma and basal cell carcinoma with greater accuracy and success. By combining cutting-edge technology with expert clinical care, patients benefit from early detection, effective treatment, and a reduced risk of recurrence. Protecting your skin, staying vigilant for new or changing lesions, and seeking prompt medical attention are key steps in maintaining your health and minimizing the impact of skin cancer.
The Path to Healing Starts With the Right Surgeon
Though board-certified dermatologists are proficient in diagnosing and dealing with a variety of ailments in the skin, Mohs micrographic surgery is a subspecialty form of expertise. It is a method involving one-stage excision with immediate frozen-section microscopic examination of the margins of tissue for ensuring maximum removal of cancer while leaving as much normal skin in its place as possible. Such a level of accuracy is particularly essential for tumors in cosmetically and functionally sensitive sites such as the face, nose, eyelids, lips, and ears, especially when treating a malignant tumor. If not fully removed, tumors can affect both the appearance and function of these areas.
Fellowship-trained Mohs surgeons are thoroughly educated in dermato-pathology, cancer surgery, and reconstruction of complex problems so their patients enjoy superior cure rates with minimal scarring and disability. By integrating cancer destruction with immediate reconstruction repair by means of local flaps and grafting, their expertise allows for restoring health in addition to aesthetics. To patients, it means not only trust in complete excision of their skin cancer but also confidence in obtaining the most natural-appearing cosmetic result. If cancer cells can break away from the primary tumor, they may spread to other areas, making complete excision critical. Don’t leave your health up to chance, seeing the right specialist is critical. Scheduling a consultation with a Mohs surgeon will give the highest cure rate and the best long-term cosmetic outcomes when treating skin cancer. Early intervention matters, be sure to book as soon as possible.






















